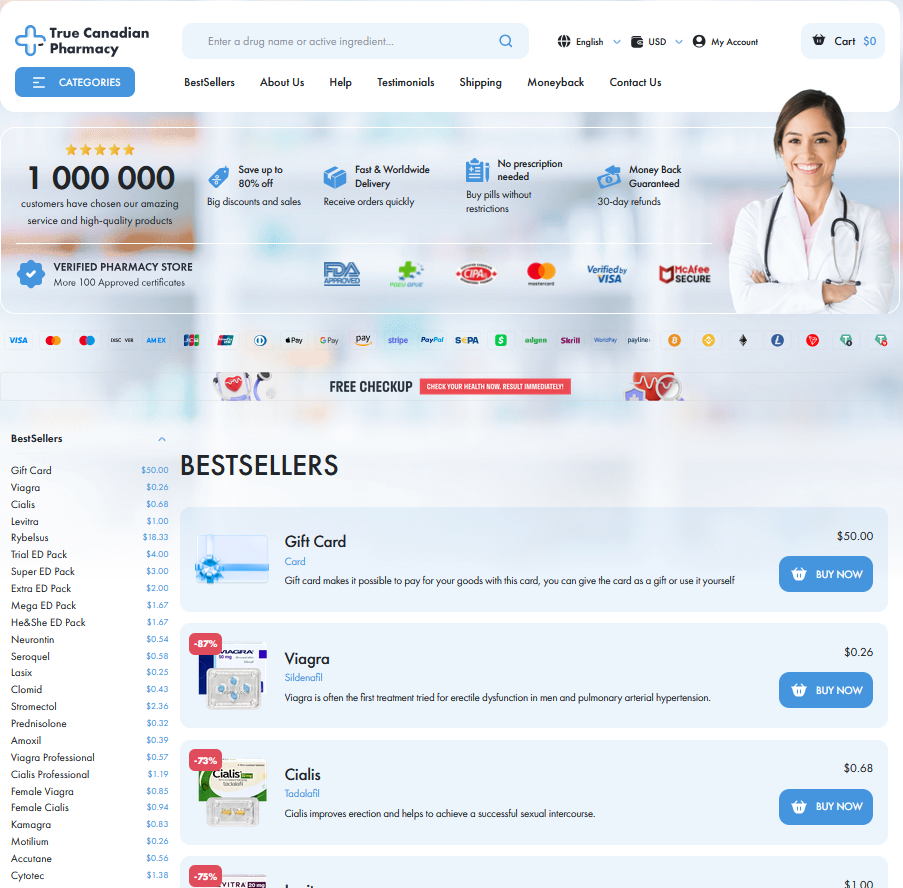
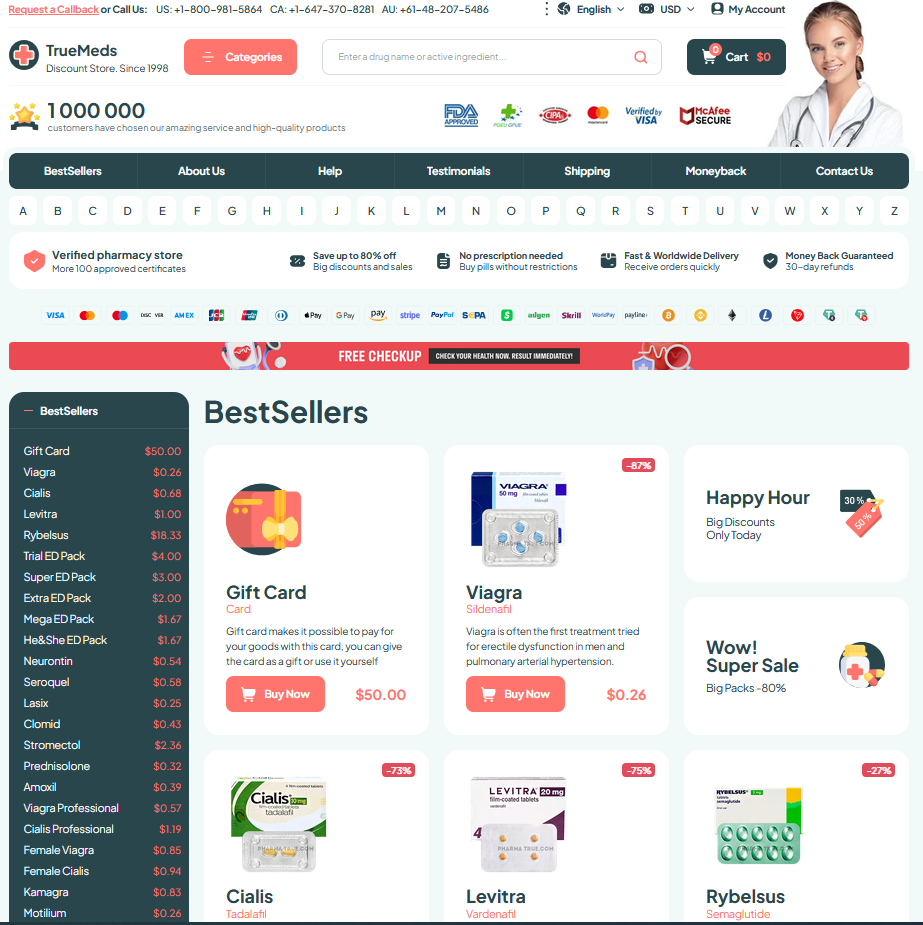
Understanding Cytotec: Its Medical Use in Obstetrics
Cytotec, known by its generic name misoprostol, has carved out a significant role in obstetrics due to its efficacy and versatility. Originally approved for treating gastric ulcers, its off-label use in obstetrics is primarily focused on inducing labor and managing postpartum hemorrhage. This synthetic prostaglandin analog helps in ripening the cervix, promoting uterine contractions, and reducing bleeding risks. Despite its practical benefits, Cytotec's journey from ulcer treatment to labor induction illustrates an intriguing medical evolution, making it a pivotal subject of both clinical and ethical discussions.
| Aspect | Description |
|---|---|
| Generic Name | Misoprostol |
| Initial Use | Gastric Ulcers |
| Obstetric Use | Labor Induction, Postpartum Hemorrhage Management |
The Mechanism of Action: How Cytotec Works

Cytotec, known generically as misoprostol, plays a critical role in obstetrics through its unique mechanism of action. It is a synthetic prostaglandin E1 analog, which interacts with prostaglandin receptors in the uterus. By binding to these receptors, Cytotec induces the uterus to contract, facilitating the cervical ripening process. This action increases the intracellular calcium levels within uterine muscle cells, igniting contractions. These contractions lead not only to the dilation and effacement of the cervix but also initiate labor. As a cost-effective and widely available medication, Cytotec’s mechanism underpins its ability to support labor induction while highlighting the need for meticulous dosing protocols to minimize potential adverse reactions.
Benefits of Cytotec in Labor Induction
Cytotec, a brand name for misoprostol, plays a transformative role in modern obstetric care by aiding labor induction. It works effectively by softening the cervix and triggering uterine contractions, making it a favored choice for healthcare providers. The efficiency of Cytotec allows for more predictable labor progressions, potentially leading to reduced cesarean section rates. Additionally, its ease of administration and cost-effectiveness make it accessible in diverse healthcare settings. Despite ongoing debates, the benefits it offers to managing labor induction remain substantial.
Safety Concerns: Weighing Risks and Side Effects

For many, Cytotec represents a medical breakthrough, yet its use in obstetrics is not free from controversy. One of the primary safety concerns revolves around the potential for uterine hyperstimulation. This condition can lead to excessive uterine contractions, which may result in fetal distress, uterine rupture, or even emergency cesarean section. Understanding these risks is crucial for healthcare professionals when considering its use.
Another layer to consider is the dosage variability that can lead to adverse outcomes. Unlike other drugs with standardized labor induction protocols, Cytotec's dosing can be unpredictable, potentially increasing the risk of complications. This unpredictability raises concerns regarding both maternal and fetal safety.
Despite these risks, many obstetric practitioners still advocate for Cytotec when used under controlled conditions. Its benefits include being a cost-effective option for labor induction. However, the decision to use it requires a thorough risk-benefit analysis by healthcare providers, with informed consent from the patients, highlighting the need to balance its promising outcomes with potential hazards.
Legal and Ethical Debates Surrounding Cytotec
Cytotec, known for its efficacy in labor induction, sparks significant legal and ethical debates. One critical discussion point revolves around the off-label use of Cytotec for inducing labor. Though it is a common practice, this usage lacks FDA approval, raising concerns about regulatory oversight. Legal challenges often arise when adverse effects occur, prompting intense scrutiny from medical boards and increasing litigation risks for healthcare providers. Ethical concerns also emerge, as informed consent becomes paramount; patients must fully understand potential risks and alternatives.
The tension between medical necessity and ethical practice is encapsulated in the practices surrounding Cytotec. While it offers a cost-effective and practical solution, questions about appropriate administration and patient safety remain. Ensuring that healthcare providers are well-informed mitigates ethical dilemmas and fosters trust between medical professionals and patients.
```html
| Aspect | Details |
|---|---|
| Legal Issues | FDA non-approval for labor, litigation risks |
| Ethical Concerns | Informed consent, patient safety |
Real-world Applications: Case Studies and Experiences
In a bustling urban hospital, Dr. Lena faced a challenging case with a patient exhibiting stalled labor. She opted for Cytotec, aware of ongoing debates yet focusing on its efficacy. Within hours, the patient progressed smoothly to delivery, illustrating Cytotec's potential when used judiciously. However, a rural clinic's story contrasts sharply; a miscalculation led to complications, reinforcing the need for skilled monitoring and application. These cases underscore both the promise and peril inherent in Cytotec use, demanding informed judgment from medical professionals and emphasizing the importance of tailoring practices to individual patients' needs for optimal outcomes.
Learn more at NCBI Read further insights on SAGE Journals